The Role of Ciprofloxacin in Fighting Bacterial Infections
Ciprofloxacin (Cipro) is a dominant, broad-spectrum fluoroquinolone antibiotic commonly suggested for critical or hard-to-treat bacterial infections. It was modified to combat bacteria that no longer respond to older antibiotics, making it especially valuable in certain complex medical situations. Cipro is used to treat a wide range of conditions from complicated urinary tract infections (UTIs) and kidney infections (pyelonephritis) to more serious issues like bone and joint infections, anthrax exposure, and difficult intra-abdominal infections. Because it is such a strong antimicrobial drug, doctors use it carefully and selectively, following modern antibiotic-stewardship guidelines to help prevent resistance and ensure patient safety. For users of our medicinesight platform, understanding both the impressive effectiveness of Cipro and the important precautions that come with it is essential for achieving safe, successful treatment results.

How Ciprofloxacin Works and Why It’s So Effective?
Ciprofloxacin is a bactericidal antibiotic, which means it does not just stop bacteria from growing it actively kills them. It works by targeting the bacteria’s DNA replication system, a process essential for their survival. Cipro blocks two key bacterial enzymes DNA gyrase and topoisomerase IV which are responsible for unwinding and copying bacterial DNA. When these enzymes are inhibited, the bacteria cannot properly repair or replicate their DNA. This leads to DNA damage, stops cell division, and finally causes the bacteria to die rapidly.
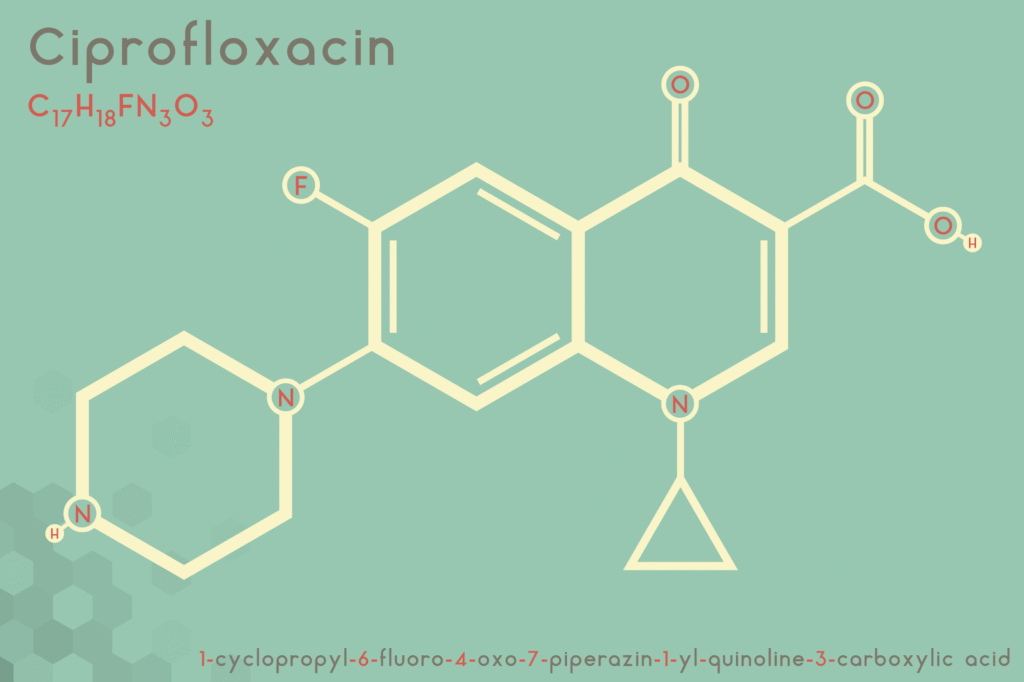
This targeted action makes Ciprofloxacin especially effective against many Gram-negative bacteria, including Escherichia coli (E. coli) the leading cause of urinary tract infections as well as Pseudomonas aeruginosa and Klebsiella pneumoniae.
Dosage and Administration How to Utilize Ciprofloxacin
Getting the dose right and following the administration instructions closely are essential for both the effectiveness and safety of Ciprofloxacin. The exact dosage depends on several factors, including the type of infection, how severe it is, where it is located in the body, and the patient’s kidney function.
| Infection Type | Recommended Oral Dose (Immediate-Release) | Duration |
| Acute Uncomplicated UTI (Cystitis) | 250 mg every 12 hours (twice daily) | 3 days |
| Complicated UTI / Acute Pyelonephritis | 500 mg every 12 hours (twice daily) | 7 to 14 days |
| Bone and Joint Infections | 500 mg to 750 mg every 12 hours (twice daily) | 4 to 8 weeks |
Administration Instructions
Timing:
Ciprofloxacin tablets or liquid suspension can be taken with or without food.
Avoid Certain Foods and Drinks:
Do not take Cipro at a time as dairy products (such as milk or yogurt) or calcium-fortified juices. These can significantly reduce how much of the medication your body absorbs. Keep a gap of at least 2 hours before or 6 hours after your Cipro dose when consuming these items.
Interactions with Antacids and Supplements:
Products containing calcium, aluminum, magnesium, iron, or zinc such as antacids, iron tablets, zinc supplements, or sucralfate (Carafate) can bind to Ciprofloxacin and block its absorption. These should also be taken 2 hours before or 6 hours after Cipro.
Hydration:
Drink plenty of fluids while taking Ciprofloxacin. Staying well-hydrated helps prevent crystal formation in the urine (crystalluria), a rare but possible side effect.
Finish the Full Course:
Even if you start feeling better, it’s necessary to complete the entire prescribed course. Stopping early can cause the infection to return and increases the risk of antibiotic resistance.
The FDA Black Box Warning: Important Safety Information
Because Ciprofloxacin relates to the fluoroquinolone class, it carries an FDA Black Box Warning the powerful safety warning issued for prescription medications. This alert highlights the risk of serious, sometimes permanent side effects. For this reason, Cipro should only be used for normal infections (like acute sinusitis, acute bronchitis flare-ups, or simple UTIs) when no safer, effective alternatives are available.
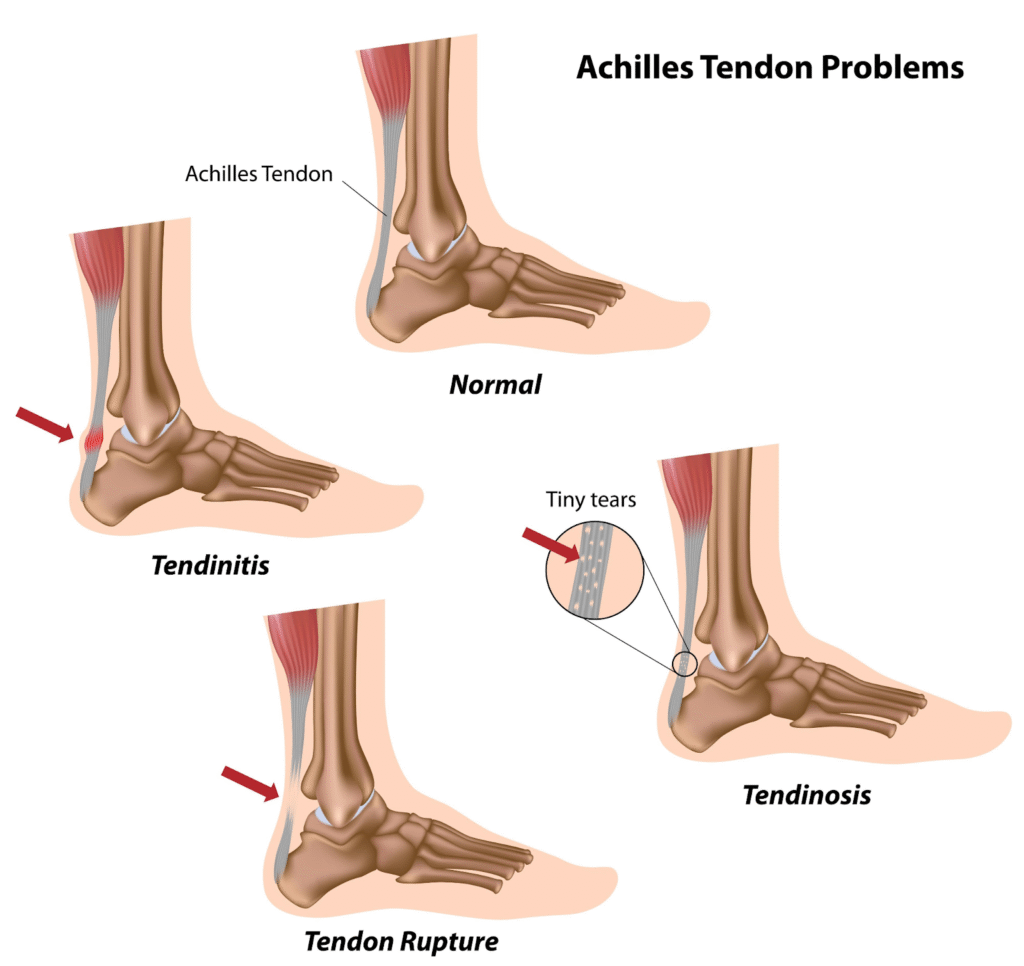
Tendinitis and Tendon Rupture
Ciprofloxacin can increase the risk of tendon inflammation and even tendon rupture, especially in the Achilles tendon. Older adults (over age 60), people taking corticosteroids, and transplant recipients are at higher risk.
If a patient experiences sudden pain, swelling, bruising, or hears a “pop” or snapping sensation in a tendon, they should stop taking Cipro immediately and seek medical attention.
Peripheral Neuropathy
Ciprofloxacin can sometimes cause nerve damage that leads to symptoms such as pain, burning, tingling, numbness, or weakness in the arms, hands, legs, or feet. In some cases, these effects may be long lasting.
Central Nervous System (CNS) Effects
Some people may experience changes in mood or behavior while taking Cipro. These can include confusion, restlessness, anxiety, hallucinations, depression, or even suicidal thoughts. Seizures (a sudden burst of electrical activity in the brain) are rare but possible.
Worsening of Myasthenia Gravis
In patients with myasthenia gravis, a condition that causes muscle weakness, Ciprofloxacin can make symptoms worse. This medication should be avoided in these individuals whenever possible.
Aortic Aneurysm and Dissection
Although uncommon, Cipro has been linked to an increased risk of dangerous tears in the aorta. This risk is higher in people with a history of aneurysms or certain genetic disorders. Sudden, severe chest, back, or abdominal pain requires immediate emergency medical attention.
Managing Common Side Effects and Drug Interactions
Aside from the serious risks, many patients experience mild and more common side effects while taking Ciprofloxacin. These usually involve the digestive system and may include nausea, vomiting, diarrhea, or stomach discomfort.
Other Important Side Effects
Clostridium difficile–Associated Diarrhea (CDAD):
Like many antibiotics, Cipro can upset the natural balance of bacteria in the gut. This may lead to an overgrowth of C. difficile, causing severe, persistent diarrhea. If this occurs, patients should seek medical care right away, as specialized treatment is required.
Photosensitivity:
Ciprofloxacin can make your skin more sensitive to sunlight. Patients should avoid excessive sun exposure and tanning beds, and use sunscreen and protective clothing while taking the medication.
QT Prolongation:
Cipro may affect the heart’s electrical rhythm, potentially causing a rare but serious condition called Torsades de Pointes. Patients with existing heart problems or low potassium/magnesium levels should use this drug with caution.
Key Drug Interactions
Ciprofloxacin can interfere with several medications by slowing their breakdown in the liver, which may cause dangerously high levels in the bloodstream. Notable interactions include:
Tizanidine (Zanaflex):
This combination is strictly contraindicated because Cipro can drastically increase tizanidine levels, leading to dangerously low blood pressure and severe sedation.
Theophylline:
Cipro can significantly raise theophylline levels, increasing the risk of severe toxicity, including seizures and cardiac complications. Blood level monitoring is essential when these drugs are used together.
Warfarin (Coumadin):
Ciprofloxacin can enhance warfarin’s blood-thinning effect, raising the risk of bleeding. Patients must have their INR checked frequently.
Methotrexate:
Cipro may increase methotrexate concentrations in the body, which can lead to toxicity.
Special Populations and Responsible Use of Antibiotics
Ciprofloxacin (Cipro) must be prescribed with extra caution in certain groups of patients. Because the drug is mainly cleared through the kidneys, people with reduced kidney function often need a lower dose to prevent the medication from building up in the body. Older adults are also more vulnerable to tendon problems and heart rhythm issues (like QT prolongation), so close monitoring is essential.
In children, Cipro is typically used only when absolutely necessary, usually for severe or complicated infections where safer alternatives won’t work, such as complicated urinary tract infections or post-exposure treatment for inhalation anthrax.
The Role of Antibiotic Stewardship
Antibiotic stewardship is a worldwide effort to ensure antibiotics are used wisely. For ciprofloxacin, responsible prescribing includes:
- Confirming the cause of infection: Using culture results and susceptibility tests to make sure Cipro is the right choice.
- Keeping treatment short and effective: Choosing the minimum duration needed for recovery (for example, 3 days for uncomplicated UTIs).
- Reserving Cipro for the right situations: Avoiding its use for viral infections or mild bacterial illnesses where safer first-line medications like nitrofurantoin or trimethoprim-sulfamethoxazole work well.
The Importance of Clear Patient Counseling
Ciprofloxacin is a powerful antibiotic and plays an important role in treating serious infections when used correctly. Its broad activity makes it highly effective, but because it comes with a number of significant risks, patients must be thoroughly informed.
Healthcare providers should counsel patients on:
- Warning signs such as tendon pain, numbness, burning, or mood/behavior changes
- When to stop the medication immediately
- How to take the medication properly and safely
Striking the right balance between the strong benefits of Cipro and its potential side effects is an essential part of modern, patient-focused care. Always speak with your doctor or pharmacist for individualized guidance, especially regarding dosing, side effects, and whether Cipro is appropriate for your condition.
Questions & Answers: Helpful Insights for Patients and Researchers
Q: Why isn’t Ciprofloxacin considered a first-line treatment for uncomplicated UTIs anymore?
A: Cipro is generally avoided for simple UTIs because of rising antibiotic resistance and important safety concerns. Overuse has made some bacteria less responsive to it, and the FDA’s Black Box Warnings highlight the risk of serious, sometimes permanent side effects—such as tendon tears and nerve damage. Because safer options exist, Cipro is now reserved for more complicated or severe infections.
Q: How long after taking Cipro can a tendon rupture happen?
A: A tendon rupture can occur while you’re still taking the medication or even months after finishing the course. It’s important to watch for tendon pain, stiffness, or swelling long after treatment is over.
Q: Can Ciprofloxacin affect my mood or mental health?
A: Yes. Cipro can trigger significant central nervous system (CNS) reactions, including confusion, agitation, paranoia, memory problems, and rarely, suicidal thoughts. These effects can appear after just one dose. Stop the medication and seek medical help right away if you notice any unusual changes in mood or behavior.
Q: Does Cipro work against viral infections like the flu?
A: No. Ciprofloxacin only fights bacteria not viruses. It won’t help with the flu, common cold, COVID-19, or any other viral illness. Using it unnecessarily can also contribute to antibiotic resistance.
Q: What should I do if I miss a dose of Cipro?
A: Take the missed dose as soon as you remember unless your next dose is coming up within the next few hours (around 6 hours or less). If that’s the case, skip the missed dose and continue with your regular schedule. Don’t take two doses at once.

Leave a Reply